Non ci sono recensioni
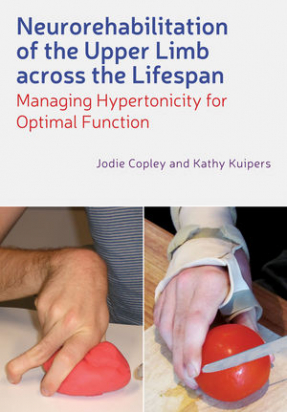
DESCRIPTION
- A comprehensive guide to managing spastic hypertonia after brain injury and the first full overview of this area
- The ideal reference for therapeutic interventions that optimise arm and hand function to support goal achievement
- An extensive clinical manual for neurological practice, a key reference for students and qualified practitioners, and a valuable resource for all occupational therapists and physiotherapists working with brain-injured clients
TABLE OF CONTENTS
Acknowledgements, ix
1. Seeing the Bigger Picture: Using Clients’ Experiences to Shape Clinical Practice, 1
1.1. Appreciating the client’s experiences, 1
1.2. Providing or assisting access to long-term services, 1
1.3. Initiating and supporting transitions from one service to the next, 3
1.4. Listening carefully and providing relevant information, 4
1.5. Collaborating on achievable goals, 5
1.6. Actively supporting and involving caregivers, 6
1.7. This book: Promoting collaborative, client-centred intervention, 7
References, 7
2. What Happens to the Upper Limb After Brain Injury?, 9
2.1. Motor control and normal movement, 9
2.2. Upper limb movement, 17
2.3. Brain injury and movement dysfunction, 19
2.4. Upper motor neuron syndrome, 20
2.5. The clinical picture: Interaction of positive and negative features, 37
2.6. Summary, 45
References, 45
3. The Hypertonicity Intervention Planning Model for Upper Limb Neurorehabilitation, 54
3.1. Decision-making in clinical practice, 54
3.2. Evidence-based practice:What it is and what it isn’t, 56
3.3. Clinical reasoning: A process of integration and differentiation, 61
3.4. The hypertonicity intervention planning model for upper limb neurorehabilitation, 65
3.5. Summary, 73
References, 73
4. Making Sense of the Clinical Picture, 80
4.1. The ICF as an assessment framework, 80
4.2. Gathering information, 81
4.3. Upper limb assessment, 87
4.4. Goal formulation, 107
4.5. Summary, 110
References, 111
4.A. Information Gathering Using a Concept Map Structure, 116
4.B. Upper Limb Performance Analysis (ULPA) Part 2: Comparative Analysis of Performance – Motor (CAP-M), 117
4.C. Upper Limb Hypertonicity Assessment Form, 119
5. Case Studies, 128
5.1. Wendy, 128
5.2. Harry, 134
5.3. Tony, 138
5.4. Summary, 144
6. Movement and Strength Training, 145
6.1. Changes in rehabilitation theory and practice, 145
6.2. Common rehabilitation approaches: Assumptions, principles and strategies, 146
6.3. A selection of contemporary techniques: Indications and considerations, 149
6.4. Summary, 176
References, 177
7. Splinting, 186
7.1. Splinting: Proposed mechanisms of effect, 186
7.2. Splinting research: A narrative review, 190
7.3. Hypertonicity intervention planning model (HIPM): Indications for splinting, 202
7.4. Splint prescription, 202
7.5. Common splint designs, 213
7.6. Adapting splint designs, 214
7.7. Commercially-produced Splints, 214
7.8. Wearing schedules, 216
7.9. Fabrication principles, 218
7.10. Summary, 223
References, 223
7.A. Common Splint Designs, Patterns and Fabrication Instructions, 230
7.B. Splint Care and Precautions, 274
7.C. Example of a Photographic Splint Programme, 275
8. Casting, 278
8.1. Casting classification, 278
8.2. Casting research: A narrative review, 282
8.3. Indications for casting, 284
8.4. Contraindications for casting, 284
8.5. Casting considerations, 290
8.6. Casting process, 294
8.7. Post-casting follow-up programme, 298
8.8. Summary, 301
References, 301
8.A. Casting Procedures, 304
8.B. Casting for Arms and Hands: Information Sheet, 316
8.C. Casting Agreement, 317
8.D. Casting Documentation Form Page 1, 318
8.D. Casting Documentation Form Page 1, 319
8.E. Precautions and Cast Care During Casting Series, 320
9. Botulinum Neurotoxin, 321
9.1. Clostridium botulinum, 321
9.2. Mechanism of effect, 323
9.3. Botulinum neurotoxin research: A narrative review, 326
9.4. Guidelines for practice, 329
9.5. Summary, 335
References, 335
10. Surgery, 339
10.1. Classification of surgical procedures, 339
10.2. Surgery: A narrative review, 340
10.3. Indications for surgical intervention, 347
10.4. Surgical consultation: Information sharing, 350
10.5. Post-surgery follow-up, 351
10.6. Summary, 352
References, 352
11. Case Studies Revisited, 355
11.1. Wendy – intervention process and outcomes, 355
11.2. Harry – intervention process and outcomes, 360
11.3. Tony – intervention process and outcomes, 362
11.4. Summary, 366
Index, 369